Camp is a great way for kids to improve their social skills, exercise, and explore new things.
If you are considering sleep away camp, but aren't sure if it's the right thing to do, click here for a psychologist's perspective on camps away from home.
Whether you decide on day camp or sleep away fun, here are some tips to get ready:
Day to Day
Sunscreen
Lather up your child with a full shot-glass worth of sunscreen every morning. Then send them to camp with a sunscreen stick, so they can reapply it as needed throughout the day (especially before and after water activities, and at lunch time). Get new tubes of sunscreen every year, and pay attention to expiration dates. Sunscreen should be thrown out 1 year after it is opened. Any sunscreen you use should be SPF 30 to 50. For more information on sunscreen choices, click here. A hat and clothing are also good ways to protect your child from harmful rays.
Insect Repellent
If your child will be in an area with mosquitos or ticks, don't forget the insect repellant. These only need to be applied once a day. If there are deer ticks in the area, please do a tick-check daily to make sure none are taking a ride, especially in the hairline. Ticks usually have to be attached to the skin and feeding for 24-48 hours before they transmit diseases like Lyme Disease, so a daily tick check can really prevent your child from getting sick. If you do find a tick, pull it out completely with tweezers, or follow the tips at HealthyChildren. Do not apply vaseline and do not burn the tick, as this can cause the tick to vomit into the host and transmit disease. For more information on insect repellants in kids, click here (Tara Haelle talks about the latest science and studies on types of repellents) and here (Dr. Iannelli discusses what to buy).
Food
If your child is going to a day camp, don't forget ice water and healthy snacks and lunch, for maximum energy and hydration. At sleep-away camp, food in the cabins can attract bugs, so it's better to leave it at home.
Safety
Teach your child to swim before they go to a camp with a pool or lake. Empower them to be protective of their body, and not to allow unwanted touches. For more help with that, see here and here. Finally, remind them to wear helmets for certain sports (rock climbing, skateboarding, bicycling, and horseback riding are popular camp activities).
Help From Your Pediatrician
Forms
Most camps require health forms to be completed by your primary care physician before you can attend camp. If you have had an annual physical office visit less than a year from the form due date, most offices will complete your forms without a visit. Some camps require the forms to be completed with a doctor's visit after April, in which case you should make an appointment as soon as possible. Either way, you will need to contact your PMD office well in advance of when you need the forms completed. Some camps are now also requiring immunization records. If you have an up to date yellow immunization card you can give the camp a copy. If you don't have one, get a copy from your pediatrician (it's a good idea to have these at all times anyways).
Medications
If your child will need to take any medications at camp, even over the counter ones, get the medication forms from camp and send them to your prescribing physician at least a couple of weeks before they need to be submitted. You should also speak to your doctor about prescribing extras for camp, especially inhalers and spacers. If your child has asthma, or wheezes, send a copy of their Asthma Action Plan to the camp.
Allergies & Special Diets
If your child has real allergies or medical diets (like with celiac disease), inform the camp ahead of time, and call to make sure they can accommodate your child safely. Allergy warning bracelets can help avoid accidental ingestion at camp, by reminding staff before they share food or special camp treats. If your child has a possibly anaphylactic (life threatening) allergy to insects, food, or anything, be sure to send an Epi-Pen or Epi-Pen Jr set (2 pens in case of anaphylaxis, not just 1) to the camp. You should also have an allergy plan, so the camp (and you) knows when to use the pen. You may need extra forms to be filled out, to be able to have these used at camp, and an extra prescription, so call your primary care or allergy doctors' office at least a month before camp starts to have this done. Teaching your child the symptoms to look for, and how to use the epinephrine is also important.
You can read more about creating a healthy camp experience at the AAP's parent site, but most importantly, have a fun summer!
Medical Mom & Kid Series
Monday, February 29, 2016
Thursday, November 5, 2015
Car Safety
Motor vehicle injuries are the leading cause of preventable death and disability in children in the USA. Using the right car seat the right away can prevent your child from getting hurt!
Vehicle Safety Information & CarSeat Review Sites:
The CDC
The CarSeat Lady (PICU mommy doctor who specializes in car safety)
CarSeats For the Littles
The CarSeat Blog
Safe Kids Worldwide
Bureau of Highway Safety
NTHSA Car Safety
The Biggest Mistakes Parents Make:
1) Not installing the carseat properly
Most parents think they have installed the car seat correctly themselves, but 71% of car seats are not installed or used correctly!
The best thing to do is have your car seat installed and checked by a certified professional. You can find car seat inspection locations here and here.
You can get advice on how to install all types of car seats here.
2) Putting the baby/child in with straps too loose, too high or low, and the chest clip not at the chest
Many parents place their child in the seat, but leave the chest clip too low and/or the straps too loose. The Car Seat Lady has a nice video explaining how to get your new infant in the seat just right. Remember, the chest clip should always be at armpit level. See above graphics (borrowed from the internet) for more information.
3) Turning a toddler forward facing too soon
Children should be at least 2 years old and have reached the maximum weight or height for rear-facing in their chair, before being turned around. Regardless of age or size, it is 5 times safer to be rear-facing!!
This video demonstrates why kids under 2 years old are in greater danger when facing forward in a crash.
This blog post by Dr. Stuppy is my favorite explanation on why kids should be rear-facing and stay in car seats as long as possible.
This website goes over common car seat direction myths.
4) Putting a child in a booster, instead of a car seat, too soon
Parents often want to move their kids to booster seats as soon as possible, for the convenience of having a lighter, more portable, cheaper seat, but it's NOT convenient if your child is hurt in a minor accident because you moved them too soon (and it will cost you a lot more money than a new car seat, too).
Children will always be safer in a 5 point restraint (aka harness system), than using a regular seat belt. I often remind my patients that race car drivers use a harness system, and don't rely on simple seat belts to keep them safe.
More information on how to decide when your child can move to a booster can be found on CSFTL and TheCarSeatLady.
5) Letting the child use a regular seatbelt too soon
This is also a matter a cost and convenience, as well as peer pressure, but don't let what other people do put your child at risk. Most children need to ride in a booster seat until at least age 10, since they need to be at least 57" (4 foot 9) to fit with a regular seatbelt. TheCarSeatLady has another good explanation on how and why booster seats work. Aside from height, they also need to be mature enough to sit straight and still i the car, since if they are leaning over in a crash, the seatbelt will not be in the proper place, and may not protect them as well as it can.
6) Letting a child/tween sit in the front seat
Children that are not fully skeletally mature (e.g. have not gone through puberty yet), and are younger than 13 years, should not sit in the front seat. Dr. Burgert does the best job explaining why on her blog. Regardless of age, size, or type of seat, everyone is safer in the back seat.
Vehicle Safety Information & CarSeat Review Sites:
The CDC
The CarSeat Lady (PICU mommy doctor who specializes in car safety)
CarSeats For the Littles
The CarSeat Blog
Safe Kids Worldwide
Bureau of Highway Safety
NTHSA Car Safety
 |
| My tall 7 year old son, very comfortable in his full car seat, making a silly face |
The Biggest Mistakes Parents Make:
1) Not installing the carseat properly
Most parents think they have installed the car seat correctly themselves, but 71% of car seats are not installed or used correctly!
The best thing to do is have your car seat installed and checked by a certified professional. You can find car seat inspection locations here and here.
You can get advice on how to install all types of car seats here.
2) Putting the baby/child in with straps too loose, too high or low, and the chest clip not at the chest
Many parents place their child in the seat, but leave the chest clip too low and/or the straps too loose. The Car Seat Lady has a nice video explaining how to get your new infant in the seat just right. Remember, the chest clip should always be at armpit level. See above graphics (borrowed from the internet) for more information.
3) Turning a toddler forward facing too soon
Children should be at least 2 years old and have reached the maximum weight or height for rear-facing in their chair, before being turned around. Regardless of age or size, it is 5 times safer to be rear-facing!!
This video demonstrates why kids under 2 years old are in greater danger when facing forward in a crash.
This blog post by Dr. Stuppy is my favorite explanation on why kids should be rear-facing and stay in car seats as long as possible.
This website goes over common car seat direction myths.
4) Putting a child in a booster, instead of a car seat, too soon
Parents often want to move their kids to booster seats as soon as possible, for the convenience of having a lighter, more portable, cheaper seat, but it's NOT convenient if your child is hurt in a minor accident because you moved them too soon (and it will cost you a lot more money than a new car seat, too).
Children will always be safer in a 5 point restraint (aka harness system), than using a regular seat belt. I often remind my patients that race car drivers use a harness system, and don't rely on simple seat belts to keep them safe.
More information on how to decide when your child can move to a booster can be found on CSFTL and TheCarSeatLady.
5) Letting the child use a regular seatbelt too soon
This is also a matter a cost and convenience, as well as peer pressure, but don't let what other people do put your child at risk. Most children need to ride in a booster seat until at least age 10, since they need to be at least 57" (4 foot 9) to fit with a regular seatbelt. TheCarSeatLady has another good explanation on how and why booster seats work. Aside from height, they also need to be mature enough to sit straight and still i the car, since if they are leaning over in a crash, the seatbelt will not be in the proper place, and may not protect them as well as it can.
6) Letting a child/tween sit in the front seat
Children that are not fully skeletally mature (e.g. have not gone through puberty yet), and are younger than 13 years, should not sit in the front seat. Dr. Burgert does the best job explaining why on her blog. Regardless of age, size, or type of seat, everyone is safer in the back seat.
No one wants to think about getting into a car accident, especially when you're transporting your most precious cargo. But with tens of thousands of deaths from motor vehicle collisions every year, no parent can afford to take chances. The odds are reasonably high that you will be involved in some kind of car accident before your littlest one turns 18. If your children are with you, you want to have done everything in your power to reduce the risk that they will suffer serious injury, and you will demonstrate to them the importance of car safety for when they have families of their own.
Saturday, February 14, 2015
From Mom to Mom: Vaccine Science Made Simple
This is a guest post by Kimberly Mulligan, PhD from the department of biological sciences at California State University Sacramento
Hi parents! Scientist here. I decided to write a long post about vaccines to help shed some light on how vaccines work and, hopefully, bring some clarity to topics of debate. The amount of misinformation about vaccines feels a little out of control to me. And no matter what you think about vaccines, it’s tough to wade through this information without a scientific background. FYI, my science background: PhD in developmental biology from Stanford University, postdoctoral research at UCSF on the molecular basis of brain development with an emphasis on a group of genes implicated in autism and other neuropsychiatric disorders, and I just joined the faculty at CSUS this January where I teach molecular cell biology and will have a research program focused on the molecular basis of neurodevelopment and neuropsychiatric illness. Ok, on to the fun stuff. (It’s long because I wanted to be comprehensive and address all of the questions I usually get about vaccines.)
First, I ask that you read this with an open mind. Having an open mind is an integral quality of good scientists – it is the only way to objectively analyze data. (Open minds are wise minds!) I also want to add that this debate gets nasty, but in the end we all love our kids and want what’s best for them (as a mama of two, I get that). I am not judging, I do not feel that is my place as a scientist – my place as a scientist is to arm you with information and help you better understand that information.
Q: Ok, so what are vaccines? (I feel like this very basic question is often not clearly answered.)
A: Usually they are viruses or bacteria that have been modified so they cannot hurt you, but still look like pathogens to your immune system. That part is key. When a weakened pathogen (or “acelluar” pieces of a pathogen) enters your body your immune system responds by making antibodies that will bind specifically to that pathogen, and target it for destruction. Here’s the really cool part – our immune system makes cells called memory B cells that will stay in our body for a really long time (depending on how strong the vaccine is). These memory B cells are primed to make antibodies specific for that pathogen if you were to get infected again. This is important because our immune response can take a long time - long enough for pathogens to have debilitating and sometimes lethal consequences. If you have those B cells ready to go, your body makes specific antibodies that will get rid of the pathogen before it hurts you.
Q: What about the other scary sounding stuff in vaccines?
A: They are all there to make sure the vaccine stays safe and effective. And while they sound awful, they are all actually totally safe in the amounts present. For example, formaldehyde sounds scary, but did you know that it is a normal metabolic byproduct that your body produces in small amounts constantly? You produce more formaldehyde over a matter of minutes than you get from a vaccine. Another fun fact: there is 4-15 times more formaldehyde in a single apple than any one vaccine. And your body simply processes it and gets rid of it (again, it knows how since you are always producing it). Aluminum? Present in things ranging from organic pears to natural breast milk. One of the first things biochemistry students learn is that dose matters. Yes, large amounts of aluminum and formaldehyde are bad…but large amounts of water can be lethal. Oh, and mercury-containing thimerosol is no longer in early childhood vaccines because it was removed due to public outcry. However, there is still zero scientific data to suggest that thimerosol has any detrimental effects. In fact, the type of mercury in thimerosol is ethyl mercury, which is readily flushed from the body. The bad mercury that our body has a harder time getting rid of is methyl mercury (found in tuna).
Q: Why should you trust a big pharma who profits from vaccines?
A: My first answer is that you don't have to. There are a lot of scientists who have published research on the safety of vaccines that are not affiliated with big pharma and do not profit from the results of their findings. They are people like me – who became scientists because they wanted to help learn more about biology in order to diminish human suffering. We work for academic institutions, not big pharma. We ask questions without a vested interest in the answers. These are the scientists that can provide you with unbiased information. You can do a search for yourself on the largest database of scientific journals here: http://www.ncbi.nlm.nih.gov/pubmed
You will find that when you search for studies on autism and vaccines, of the hundreds of studies conducted, there is still no scientific data to suggest a link between the two. For example, every epidemiological study conducted on populations of children living in the same community has shown autism occurs at the same rate in vaccinated and unvaccinated children.
Q. What is currently thought to be the cause of autism?
A: It is currently thought that autism is a neurodevelopmental disorder that often begins in utero. A number of the autism risk genes identified affect how the brain develops during gestation. There were actually a couple of papers very recently published indicating specific mutations in a large number of candidate risk genes for autism1, 2. There has also been research showing the influence of environmental factors like maternal antibodies that are present in the womb, which were identified by scientists at the UC Davis MIND Institute3. Autism is a very complicated disorder, and we certainly don’t have all of the answers! But, again, there has been an overwhelming amount of time and money dedicated to investigating a potential link between autism and vaccines, and every study has come back with the same results: there is no data to suggest a link between autism and vaccines.
Q: Back to the big-pharma-makes-a-lot-of-money-argument.
A: Yes, they do. They make money on every drug they produce. I have opinions on big pharma’s business practices that I won’t go into now because it actually has nothing to do with the argument about vaccine effectiveness or safety. For better or for worse, our entire medical system is profit based (our entire economy is, actually). The people at the forefront of the anti-vaccination movement also make a lot of money. That is not why I don’t believe them, though. I don’t believe anti-vaccination proponents because of the absence of scientific data to support their claims. As a scientist, I only believe what the scientific data supports. I read research, not opinions. (That is not meant as a slight to anyone! I am simply stating my practices. I know that reading primary research papers can be like reading a different language if you do not have a science background, so I would not really expect any non-scientist to have this practice. It’s the same reason I don’t read economics papers. Bleh!)
Q: What about vaccine-related injury?
A: The overall risk is something like 0.003%. And the VAST majority of those 0.003% have minor allergic reactions. Severe allergic reactions can occur, though they are extremely rare. There have been a few cases of autoimmune disorders being triggered by a vaccine. It is not entirely clear whether the vaccine was actually the trigger because it could have been triggered by any pathogen. Importantly, people who are immunocompromised, meaning they have a weakened immune system (chemotherapy patients, HIV patients, genetic immune deficiencies, etc.), cannot be immunized because their immune systems are so weak that even the weakened virus might hurt them. All of these people fall into the class of people who should not get vaccinated and for whom herd immunity is so important!
Q: What is herd immunity?
A: It’s kind of basic math. Viruses cannot replicate on their own. They need to infect a host cell in order to replicate. If they don’t make it into a host cell, they will eventually die. Here's an easy example: a person infected with a virus walks into a room where there are 20 vaccinated people separating him from a single unvaccinated person. That virus cannot move from the infected person and replicate in any of the vaccinated people because once it gets into their bodies, those memory B cells start pumping out antibodies that kill it before it can replicate and spread. Therefore, those 20 vaccinated people make it harder for the virus to make it to the single unvaccinated person. If half of the people were unvaccinated, that virus would get to have a replication party in all of their cells and would have a much easier time surviving, multiplying, and spreading. Herd immunity is just a basic principle about how infectious pathogens spread. If someone tells you it doesn’t exist, you should be wary of any other scientific information they give you because it means that they have never taken or studied immunology or microbiology and are not qualified to have an educated discussion about those topics.
The tricky thing about vaccines and herd immunity is that herd immunity really only works when a high percentage of the population are vaccinated. If not, then viruses have an easier time spreading around our communities, putting at risk our neighbors who cannot be vaccinated (newborns, cancer patients, etc.), and who are also much more likely to die as a result of infection. That is why the scientific community is so scared. We feel that even a single death from a vaccine-preventable disease is a tragedy.
Q: Isn’t natural immunity better than vaccine-induced immunity?
A: Well, the immune response is stronger because the pathogens are not weakened, so if you make it through the illness you will, in theory, have a great supply of those memory B cells. The problem is that a lot of these vaccine-preventable pathogens can cause blindness, deafness, brain damage, paralysis, or death. I know of a mama who has a sister who contracted rubella while she was pregnant. Her baby was born blind and deaf because of the infection. So, yes, she now has great immunity to rubella. But she would give anything to have had vaccine-induced immunity prior to her pregnancy.
Q: Why do some vaccines not give lasting immunity?
A: Each vaccine has a varying degree of effectiveness. By effectiveness I specifically mean the quantity and quality of memory cells that will stick around in the immune system post-vaccine. For example, the smallpox vaccine gave immunity for 65 years whereas the pertussis vaccine only lasts for about 10 years. This is the purpose of boosters. Boosters essentially tell your immune system that it is still important to mount a defense against the pathogen, and replenishes your stock of memory cells.
Q: I heard a lot of adults are to blame for the current measles outbreak. Should adults get vaccinated, too?
A. Absolutely! If you are unsure of your immunity, you can talk to your medical provider about checking your titer (a measure of your immunity), or you can just get a booster. Even if you’ve had a booster, but can’t exactly remember when and your provider doesn’t do the titer test, getting another booster cannot hurt you.
Q: Why do babies often get fevers after being vaccinated?
A: Part of the natural immune response is the release of molecules called chemokines, which cause fever. As a mama, I know how scary it can be when your little one has a fever, but a post-vaccine fever is indicative of a robust immune response and means they are making great memory B cells. That does not mean you shouldn’t treat your baby’s fever! (Please consult your pediatrician on when you should treat your baby’s fever.)
Q: What’s up with vaccine shedding?
A: Vaccine shedding is something only possible with a live attenuated virus. This is different from the pertussis vaccine, for example, which is an acellular vaccine, meaning it contains various pieces of the pertussis bacterial molecules and is not infectious at all, cannot cause illness ever, and cannot shed. Again, a live attenuated virus is a weakened virus that reproduces so slowly that a normal immune system will take care of it before it causes any harm. If a person is immunocompromised, live attenuated vaccines cannot be used because their immune system might not be able to handle even a weakened virus. The nasal spray flu vaccine does have a risk of vaccine shedding because the vaccine is administered directly to the mucus membranes of the nose. Therefore, if that recently immunized person were to sneeze onto an immunocompromised person, there is a theoretical possibility that the attenuated virus could give that immunocompromised individual the flu. This is why it is recommended to stay away from immunocompromised individuals for a week after getting the nasal spray flu vaccine. Other live attenuated viruses are injected into muscle. Some of the weakened virus will get into the lymphatic system, which is where all that good immunity will happen (production of specific antibodies, effector cells, and memory cells that will stay around for a long time). From there, some of the vaccine can enter saliva and mucus, although it is going to be a much lower amount. I think this is why the CDC only has the recommendation to steer clear of immunocompromised individuals in the case of the nasal spray flu vaccine. BUT, and this is critical, the virus that would potentially be shed post-vaccine is the attenuated (weakened) virus that does not cause illness in a person with a normal immune system. This is why vaccine shedding does not cause disease EVER in a person with a normal immune system. It would essentially be like getting an ultra-tiny dose of a vaccine (not enough to even cause an appreciable immune response that would lead to acquired immunity). This is anecdotal, but when my daughter was newborn, my husband did not realize this about the nasal spray flu vaccine when he took our 2 year-old to the doctor…and he got him the nasal spray form of the flu vaccine. I’m happy to report that my newborn daughter did not get the flu. I actually wasn’t really worried; it’s a very minimal risk….but when a person is severely immunocompromised it is important to worry about any potential risk.
Q: If I have a baby that is too young for MMR, could a booster given to a breastfeeding mama give the baby passive immunity through antibodies present in the breast milk?
A: Passive immunity is the transfer of active antibodies from one person to another. This happens during pregnancy when antibodies present in mama cross the placenta to the developing fetus. I recently spoke to an immunologist friend about passive immunity through breast milk. I myself was considering getting the MMR booster to help my 7 month-old baby girl, but he said (sadly) it probably would not boost her passive immunity an appreciable amount (for a virus as strong as measles, anyway). There are five classes of antibodies (IgA, IgG, IgD, IgE, and IgM). The type that is most effective in preventing infection from something like the measles is IgG. These antibodies cross the placenta during pregnancy and give passive immunity to the baby when it is newborn. The primary type of antibody that gets into breast milk is IgA. It provides some protection, but it’s just not as great as IgG.
Q: If newborns get passive immunity from mama during pregnancy, why are they susceptible to illness?
A:Passive immunity only lasts for a short time. That’s because antibodies tend to not survive very long (a few weeks to a few months, on average). Unfortunately, the effector cells and memory cells that are responsible for making the antibodies in mama do not cross the placenta. The memory cells are the cell types that stick around for years to provide lasting immunity. I read a study that indicated 88 percent of babies of vaccinated mothers have passive immunity to measles at 4 months, and that number dropped to 15 percent by 8 months of age4. Although, and this is important, the amount of antibodies acquired through passive immunity may not be sufficient to protect the baby from a strong pathogen.
Q: What about the alternative vaccine schedule versus the CDC recommended vaccine schedule?
A: I've never found evidence to support the alternative vaccine schedule. It is my understanding that it is something to make parents feel more comfortable. There are a lot of factors taken into account for the CDC schedule, which have to do with considerations like when the acquired immunity will be best. For example, MMR is not given until 12 months because they want to make sure that all passive immunity acquired from mama during pregnancy is gone by the time the vaccine is administered because those circulating antibodies would decrease the immune response to the vaccine. So MMR can be given at 6 months, but is better at 12 months...and I recently read a study indicating even a little tiny bit better at 15 months5; but, you could possibly do the initial shot earlier than 12 months and then get the booster early if you are concerned about measles in your community (of course, talk to your doc about these decisions).
I hope this was helpful! Again, I have no financial interest in this debate. As the mama of a 7 month-old baby girl who is not old enough to have MMR, a 2 year-old little boy who only now has partial immunity, and as the stepdaughter to a wonderful man who spent his final 9 months severely immunocompromised due to chemotherapy, I am certainly emotionally invested in the debate. But as a scientist who has read thousands of pages of scientific research, I only want to help spread knowledge and quell fear.
For links to more information about vaccines please check out this post: http://mommedicine.blogspot.com/2013/03/immunization-information.html
For links to more information about vaccines please check out this post: http://mommedicine.blogspot.com/2013/03/immunization-information.html
References
1 Iossifov I, et al., The contributions of de novo coding mutations to autism spectrum disorder. Nature. (2014) 515(7526)
2 De Rubeis S, et al., Synaptic, transcriptional and chromatin genes in autism. Nature. (2014) 515(7526)
3 Bauman MD, et al., Maternal antibodies from mothers of children with autism alter brain growth and social behavior development in the rhesus monkey. Transl Psychiatry. (2013) 9;3
4 De Serres, et al., Passive immunity against measles during the first 8 months of life of infants born to vaccinated mother or to mothers who sustained measles. Vaccine. (1997) 15(6-7):620-3.
5 Hinman A., et al., Comparison of Vaccination with Measles-Mumps-Rubella Vaccine at 9, 12, and 15 Months of Age. J Infect Dis. (2004) 189
Labels:
baby,
bacteria,
bio,
child,
immunizations,
parenting,
pediatrics,
sick,
teenager,
toddler,
travel,
vaccines,
virus
Monday, January 5, 2015
Wheezing: Tips for Kids Using Inhalers
Children with wheezing, reactive airways, asthma, bronchospasm, or difficulty breathing are often prescribed a metered dose inhaler with a spacer device.
There are different kinds of metered dose inhalers (“MDI”):
1) A “rescue inhaler” contains Albuterol or Levalbuterol, which opens up the lungs and reduces inflammation for quick relief. Brand names include Ventolin, ProAir, Proventil, or Xopenex. These are equivalent to putting 1 vial of Albuterol or Xopenex in a nebulizer and sitting with the mask on your child for 15 minutes. These are usually used on an as-needed basis, up to every 4 hours. If your child needs to use this every 4 hours for more than 24 hours, needs it more often than every 4 hours, or needs this more than twice every week, please call your pediatrician.
2) Some inhalers are used to prevent asthma, wheezing, and breathing trouble. These are only effective when used every day. They are not used for fast-acting relief of an acute breathing difficulty, but may help when used during cold or allergy season, or if started right at the beginning of an asthma exacerbation or when a child is exposed to known triggers. Brand names of some of these medicines include Flovent, Qvar, Symbicort, Dullera or Advair. Flovent and Qvar are like using the Pulmicort/Budesonide in the nebulizer. Please discuss if and when you should use these with your physician.
3) There are also inhalers that contain powder or are not used with a spacer. Some brand names are: Maxair autohaler, Asmanex Twisthaler, or Pulmicort Flexhaler. None of these need a spacer to work effectively, but these are only for older children.
Please see the “Asthma Education For Kids” playlist from BoosterShotComics on YouTube, especially episode #1: “Iggy & The Inhalers” to better understand the roles of different medications used for wheezing or asthma. Episode 4 explains how to use a spacer with mouthpiece.
There are 4 main brands of spacers. They may be cheaper online than from a pharmacy, but always require a prescription.
1) Aerochamber with flow-vu. This brand is a clear tube with colored ends and teddy bears on the side. It has a two-way valve (to get the medicine in and air out) and is anti-static (so the kid can inhale all of the medicine and it won’t stick to the sides). The flow-vu allows you to see when a child gets a breath with a good seal. There is a small orange one for infants, yellow medium one for age 1-5 years old, blue one with mask for older children that still need a mask, and blue one with mouth-piece for older kids that can seal their lips around it instead of having to use a mask (more comfortable, kids can usually start doing this around age 6).
2) Vortex Non-Electrostatic Valved Holding Chamber. This device also has a two-way valve and is anti-static. It is metal, so it is more durable and machine-washable. It comes in 1 size with different sized masks that fit on the end. This has the advantage of only needing one device as the child grows older (you just switch the mask on the end, not the whole device).
3) Optichamber. The original device is a plastic tube with 1-way valve that most pharmacies try to give our patients. Some versions are NOT anti-static, therefore much of the medicine sticks to the plastic, instead of being inhaled by the child. The single valve can make some children feel suffocated when breathing into the mask. I do NOT recommend this device. However, there is now an Optichamber Diamond version, which is anti-static, has a 2-way valve, and can be used comfortably. It comes with different size masks or a mouth piece, all clear, and very soft.
4) InspiraChamber. This is a clear, anti-static, valved chamber, with purple ends. It offers very soft masks with a special place in the small mask to fit a pacifier, to calm the child while they inhale. It also has a flap that moves, so you can see if the child is taking a breath with a good seal and getting the medicine. It will be available after February 2015.
How to Use Your Inhaler:
my son playing with his inhaler and spacer a few years ago (C) 2015
To use a spacer with a mask:
- Shake the inhaler before each use.
- Put the inhaler mouthpiece into the spacer.
- Hold the mask over your child's nose and mouth and create a good seal. Holding your fingers like the letter C can help. If you’re using a device with flow-vu, you should see the flap move with each breath the child takes. Otherwise look at the child’s chest to count breaths.
- Press the inhaler.
- Have your child breath in and out six times (about 30 seconds).
- Remove the mask and let your child breath normally for a minute.
- Repeat if more than one puff was prescribed (most inhalers need 2 puffs per dose).
While your younger child may not like the spacer and mask being held over his mouth and nose, it will go much quicker than using a nebulizer. Let the child play with it and practice putting it on stuffed animals or family members to make them comfortable. Some children will allow you to use it if they get to be the ones to hold it or press the inhaler (just make sure the seal is tight over their face so they get all of the medicine).
- Shake the inhaler before each use.
- Put the inhaler into the spacer.
- Have your child seal their lips around the mouthpiece and exhale.
- Press the inhaler.
- Have your child breath the medicine in and hold their breath for about 30 seconds. If they can’t hold their breath, they can take another breath or 2 in to get more medicine from that puff (any extra medicine should be sitting in the chamber).
- Take the spacer out of their mouth and have the child breath normally for a minute.
- Repeat if more than one puff was prescribed (most inhalers need 2 puffs per dose).
Keep in mind that while many experts believe that an MDI with a spacer is as good as, or better than, a nebulized treatment, some parents prefer a nebulizer, and that is okay.
If you are not sure if your child is actually wheezing, or what they have, this blog from Dr. Stuppy can help, with descriptions of different kinds of coughs and breathing, along with youtube video links.
If your child does NOT have asthma, reactive airway disease, wheezing, bronchospasm, or difficulty breathing, my post on Coughs, Colds and Croup may be more helpful.
Please note that this guide is NOT intended to diagnose or treat any illness or condition. Always speak to your own physician for advice.
Labels:
albuterol,
asthma,
baby,
bronchospasm,
child,
congestion,
cough,
croup,
inhaler,
medicine,
pediatrics,
reactive airway disease,
spacer,
virus,
wheezing
Tuesday, July 29, 2014
Private Parts: Talking to Your Child About Their Bodies, Behavior, and Babies
It is important to start speaking with your children about their bodies and behavior at an early age. If you create an open dialogue, without shame, your children will feel free to bring you their questions throughout their lives. This is often an uncomfortable topic for parents, so I have created a list of books and resources to help you get through it (scroll down). I also encourage you to discuss any questions you have on the topic with your child's pediatrician (we are always here to help!).
Some tips:
- Watch out for everyday opportunities to teach your child about privacy and hygiene.
- Encourage your child to ask you questions, to learn that they can feel comfortable coming to you with their thoughts.
- Try to be calm and open about the topic (pay attention to your body language and tone of voice).
- Give simple and short answers.
- Make sure your answers are age appropriate.
- Young children take everything you say literally, so avoid metaphors.
- Use anatomically correct terms for their body parts (i.e. penis and vulva, not "weewee")
- Avoid shame and ridicule.
- Become closer to your child by showing them that you accept & support their feelings.
- Set rational and consistent limits.
Here is a great blogpost by Dr. Claire McCarthy on getting started with the conversation: "6 Tips For Talking To Your Kids About Sex."
I also recommend looking at the website "Empowering Our Children," which is designed to teach parents how to protect their children from sexual abuse.
The "ScaryMommy" website has a good post on what these conversations with toddlers may look like.
The "ScaryMommy" website has a good post on what these conversations with toddlers may look like.
My Book Recommendations:
For parents to read overall:
- “Everything You NEVER Wanted Your Kids To Know About Sex (but were afraid they’d ask)” by Dr. Justin Richardson & Dr. Mark Schuster
This is the best book for parents to read on the subject. It tackles every sexual stage of development from infancy (yup, some babies masturbate) through adolescence, as well as age-less topics, such as homosexuality. I recommend starting to read this book when your child is young, although it’s never too late to learn.
For parents to read on tough questions kids ask in general (not on sex):
- “The Top 50 Questions Kids Ask” by Dr. Susan Bartell
- “Questions Children Ask & How To Answer Them” by Dr. Miriam Stoppard
These books cover tough questions that kids bring up in general, like spirituality, fear, and growing up. The first book is good for uncovering the real meaning behind some questions, and figuring out the best way to respond.
Books to read with your children (or for them to read by themselves), by age group:
Toddlers & Pre-Schoolers:
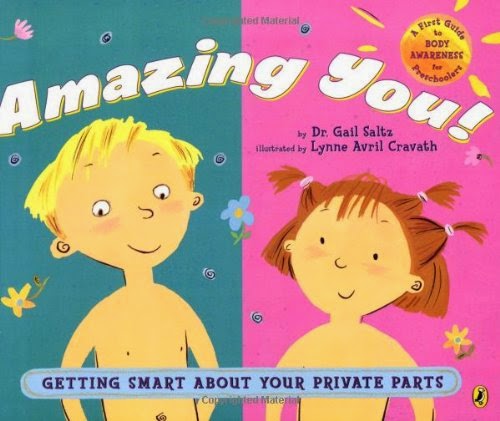
- “Amazing You: Getting Smart About Your Private Parts” by Dr. Gail Saltz
My favorite overall book for toddlers. Teaches basic anatomy, privacy, and even how babies are born.
- “When You Were Inside Mommy” by Joanna Cole
A very simple book on pregnancy and birth to read to young children. No lies (e.g the stork), but no anatomy or private parts mentioned either.
- “What Makes a Baby?” by Cory Silverberg
This book is great for families that conceived via IVF, adoption, surrogacy, or traditional means. It talks about sperm, egg, uterus, and birth, but each as its own thing, and at the end it asks, “Who was waiting for you to be born?” Technically accurate, but simple, with cartoonish illustrations.
- “Where Did I Come From?” by Peter Mayle
This is the classic “how babies are made” children’s book, but take a look through this book before buying it, as it is may be too explicit for some families (see the anecdote at the end of this blog post).
- “My Body Belongs To Me” by Jill Starishevsky
This book discusses inappropriate touching/abuse. It does not discuss development or how babies are made.
School Age Children:
- “It’s So Amazing! A Book About Eggs, Sperm, Birth, Babies, and Families” by Robie Harris
Tweens:
- “It’s Perfectly Normal: Changing Bodies, Growing Up, Sex, and Sexual Health” by Robie Harris & Michael Emberley
Very similar to the school-age version by Harris (above), but with more words, less illustrations, and more details.
- “The Care & Keeping of YOU: The Body Book for Girls” by American Girl
My tween patients report that they love this book. It goes over what to expect in puberty and how to take care of girls’ changing bodies. This book includes discussions on hygiene and how to use menstrual products. There is a new version with the number 2 on it, and a version for boys.
Dr. Stuppy and the Mighty Girl website also have good posts on discussing puberty.
An Anecdote:
When I was 3 years old, my mother (who is a pediatrician as well) read me the book "Where Did I Come From?" I went to my religious nursery school and proceeded to tell everyone, "I was the fastest sperm!" Some of the other parents were not happy when their own children went home and repeated the same thing to them. My mom got a stern 'talking to' by the school. We still laugh about it, to this day. The moral of the story? Teach your children about their bodies and development before anyone else does, or you may not be happy with what they learn ;)
For newer blog posts on the subject, as they come out, you can also follow my pinterest boards on Teenagers, Parenting, and Kids' Health.
Labels:
baby,
child,
development,
medicine,
parenting,
pediatrics,
puberty,
sex,
teenager,
toddler
Wednesday, October 2, 2013
Vomiting and/or Diarrhea
Vomiting and diarrhea viruses are not fun for anyone. Doctors refer to the most common cause of these symptoms as "viral gastroenteritis". Some kids just vomit, some kids just have diarrhea, and the most unlucky have both.
Most of these illnesses do not need to be treated with medications (antibiotics can make it worse, since they also kill the good bacteria in your tummy), and anti-diarrheal medicines (like Imodium) can be harmful to children. The most important thing is to keep your child HYDRATED (more on that below). If you suspect your child has vomiting or diarrhea from food poisoning or any other type of foreign ingestion, please call poison control 1-800-222-1222, who are free and staffed with physicians 24-7!
How can you tell if your child is starting to get dehydrated?
- their mouth/lips seem dry
- they are urinating (peeing) a little less than usual
- they are thirsty
Now what?
You need to keep your child hydrated!
- A baby can continue to breast feed or take infant formula, if they are just a little dehydrated. If they vomit after every feeding, or are refusing the breast/bottle, then try to hydrate them with an Oral Rehydration Solution, like Pedialyte. Warning: the plain ones taste like salt water, so I suggest getting a few flavored ones and trying them out, to see which ones they will take. If they refuse the bottle completely, you can try feeding them via a syringe or spoon, giving small amounts every 15 minutes.
- A child who is getting electrolytes from food (such as chicken soup, or crackers, even if it's just a little bit) can hydrate with water. If they are not taking in any food, or if they are throwing up the food, please hydrate them with an ELECTROLYTE solution (aka Oral Rehydration Solution, aka ORS). You can buy them at most USA markets (under brand name Pedialyte, or generic versions), you can make your own by mixing 1 liter (5 cups) clean water with 6 level teaspoons (=2 tablespoons) sugar and 1/2 teaspoon salt. You can add a little bit of orange juice or a banana for potassium. Common substitutions are rice water, congee, green coconut water, or mixing gatorade with water (although I do not recommend doing this, since it is hard to get the right balance of electrolytes this way). If your child does not want to drink, try giving them sips every 15-30 minutes, or giving them the ORS/Pedialyte in frozen popsicle form.
- For every age, and everybody in the house, WASH YOUR HANDS A LOT to prevent spread/transmission of the stuff that gets you sick. Teach everyone to wash their hands in warm water, scrubbing for at least 20 seconds (2 rounds of the Happy Birthday song). Try and use real soap and water, instead of no-rinse hand sanitizers, since they do a better job at killing the tummy microbes.
But what if they keep vomiting?
- Let their tummy rest.
- Call your pediatrician, or go to the hospital, if they have signs of dehydration (see more below).
- Ask your pediatrician if your child is old enough and healthy enough for a medication against nausea/vomiting.
- Start with no food, but still give an electrolyte fluid (aka ORS above), for the first 12 hours.
- When they are ready/want to eat, give bland foods (e.g. the popular rice, toast, soup) and avoid foods that are fried, acidic, oily, or contain lactose.
But what if they have icky diarrhea?
- Change the diaper or bring them to the toilet frequently. Use a LOT of diaper cream to keep the area from getting chapped/sore. Put on a zinc cream (like the purple desitin) as if you are icing a cake - this acts as a barrier layer, to prevent acidic poop from sitting on the skin.
- Feed them binding foods, like rice.
- Sometimes the microbes that cause diarrhea, also cause a temporary lactose (the sugar in cow's milk) intolerance, so avoid lactose-containing stuff, like cow's milk and cheese. You usually have to do this for 2-4 weeks after the onset of the illness, until their GI system is back to normal.
- Try a children's probiotic with lactobacillus once per day, such as children's culturelle.
When my patients get sick this way, I often refer them to the great patient resources at UpToDate, such as this one on nausea and vomiting in children:
http://www.uptodate.com/contents/nausea-and-vomiting-in-infants-and-children-beyond-the-basics?detectedLanguage=en&source=search_result&search=patient+information&selectedTitle=7~150&provider=noProvider
or this one on diarrhea in children:
http://www.uptodate.com/contents/acute-diarrhea-in-children-beyond-the-basics?source=see_link
How can you tell if your child is dehydrated enough to warrant intervention (like an urgent care or ER), or at least a call to your pediatrician?
- they are not urinating (peeing) often enough (every 4-6 hours for a baby, every 6-8 hours for a toddler/child, every 8-12 hours for an older child/adolescent)
- they are crying, but can not make tears
- they are an infant whose fontanel (soft spot on top of the head) is more sunken than usual
- eyes look very sunken
What are some other signs that I should call my pediatrician about, or head over to the local urgent care/ER?
- persistent high fever (above 102.5 F)
- any fever in an baby younger than 3 months old
- severe abdominal (tummy) pain
- abdominal pain that moves to the lower right side
- lethargy or decreased responsiveness
- bloody (red or black) or bright green (like pea soup) vomit or diarrhea
- diarrhea not improving after 1 week
The good news is that the gastroenteritis season is almost over, so hang in there. However, we are getting into cough and cold season, so see my August 2012 post for tips on that:
http://mommedicine.blogspot.com/2012/08/coughs-colds-and-croup.html)
Most of these illnesses do not need to be treated with medications (antibiotics can make it worse, since they also kill the good bacteria in your tummy), and anti-diarrheal medicines (like Imodium) can be harmful to children. The most important thing is to keep your child HYDRATED (more on that below). If you suspect your child has vomiting or diarrhea from food poisoning or any other type of foreign ingestion, please call poison control 1-800-222-1222, who are free and staffed with physicians 24-7!
How can you tell if your child is starting to get dehydrated?
- their mouth/lips seem dry
- they are urinating (peeing) a little less than usual
- they are thirsty
Now what?
You need to keep your child hydrated!
- A baby can continue to breast feed or take infant formula, if they are just a little dehydrated. If they vomit after every feeding, or are refusing the breast/bottle, then try to hydrate them with an Oral Rehydration Solution, like Pedialyte. Warning: the plain ones taste like salt water, so I suggest getting a few flavored ones and trying them out, to see which ones they will take. If they refuse the bottle completely, you can try feeding them via a syringe or spoon, giving small amounts every 15 minutes.
- A child who is getting electrolytes from food (such as chicken soup, or crackers, even if it's just a little bit) can hydrate with water. If they are not taking in any food, or if they are throwing up the food, please hydrate them with an ELECTROLYTE solution (aka Oral Rehydration Solution, aka ORS). You can buy them at most USA markets (under brand name Pedialyte, or generic versions), you can make your own by mixing 1 liter (5 cups) clean water with 6 level teaspoons (=2 tablespoons) sugar and 1/2 teaspoon salt. You can add a little bit of orange juice or a banana for potassium. Common substitutions are rice water, congee, green coconut water, or mixing gatorade with water (although I do not recommend doing this, since it is hard to get the right balance of electrolytes this way). If your child does not want to drink, try giving them sips every 15-30 minutes, or giving them the ORS/Pedialyte in frozen popsicle form.
- For every age, and everybody in the house, WASH YOUR HANDS A LOT to prevent spread/transmission of the stuff that gets you sick. Teach everyone to wash their hands in warm water, scrubbing for at least 20 seconds (2 rounds of the Happy Birthday song). Try and use real soap and water, instead of no-rinse hand sanitizers, since they do a better job at killing the tummy microbes.
But what if they keep vomiting?
- Let their tummy rest.
- Call your pediatrician, or go to the hospital, if they have signs of dehydration (see more below).
- Ask your pediatrician if your child is old enough and healthy enough for a medication against nausea/vomiting.
- Start with no food, but still give an electrolyte fluid (aka ORS above), for the first 12 hours.
- When they are ready/want to eat, give bland foods (e.g. the popular rice, toast, soup) and avoid foods that are fried, acidic, oily, or contain lactose.
But what if they have icky diarrhea?
- Change the diaper or bring them to the toilet frequently. Use a LOT of diaper cream to keep the area from getting chapped/sore. Put on a zinc cream (like the purple desitin) as if you are icing a cake - this acts as a barrier layer, to prevent acidic poop from sitting on the skin.
- Feed them binding foods, like rice.
- Sometimes the microbes that cause diarrhea, also cause a temporary lactose (the sugar in cow's milk) intolerance, so avoid lactose-containing stuff, like cow's milk and cheese. You usually have to do this for 2-4 weeks after the onset of the illness, until their GI system is back to normal.
- Try a children's probiotic with lactobacillus once per day, such as children's culturelle.
When my patients get sick this way, I often refer them to the great patient resources at UpToDate, such as this one on nausea and vomiting in children:
http://www.uptodate.com/contents/nausea-and-vomiting-in-infants-and-children-beyond-the-basics?detectedLanguage=en&source=search_result&search=patient+information&selectedTitle=7~150&provider=noProvider
or this one on diarrhea in children:
http://www.uptodate.com/contents/acute-diarrhea-in-children-beyond-the-basics?source=see_link
How can you tell if your child is dehydrated enough to warrant intervention (like an urgent care or ER), or at least a call to your pediatrician?
- they are not urinating (peeing) often enough (every 4-6 hours for a baby, every 6-8 hours for a toddler/child, every 8-12 hours for an older child/adolescent)
- they are crying, but can not make tears
- they are an infant whose fontanel (soft spot on top of the head) is more sunken than usual
- eyes look very sunken
What are some other signs that I should call my pediatrician about, or head over to the local urgent care/ER?
- persistent high fever (above 102.5 F)
- any fever in an baby younger than 3 months old
- severe abdominal (tummy) pain
- abdominal pain that moves to the lower right side
- lethargy or decreased responsiveness
- bloody (red or black) or bright green (like pea soup) vomit or diarrhea
- diarrhea not improving after 1 week
 |
| Soon your baby will be back to enjoying (throwing) his food (c) 2013 |
http://mommedicine.blogspot.com/2012/08/coughs-colds-and-croup.html)
Tuesday, May 21, 2013
Fun in the Sun:
Sunscreen Tips and Links
SPF 30-50 are best. SPFs that are higher than that do not add significantly more protection.
The safest sunscreens are barrier sunscreens. These are sunscreens that use zinc oxide or titanium dioxide as the active ingredient, which sit on the skin to provide a shield from the sun. Since they are not absorbed systemically, I recommend using only these types of sunscreens* on infants (in addition to shielding clothing and hats).
Chemical sunscreens are those that contain chemicals which are absorbed into the skin to provide protection. These are newer, but still safe when used correctly. Some of the active ingredients in chemical sunscreens include, but are not limited to, octinoxate, octocryleme, oxybenzone. Most sunscreens on the market today use these, and there are many more options that kids like with these formulations, such as sprays, colors, and different textures. The best sunscreen is the one you can actually get on your child everyday. The aerosol spray sunscreen versions should only be used outside, in well ventilated areas, and below the neck, because they are meant to be sprayed evenly on the skin (you should see a layer of sunscreen forming), and not breathed in. They are a quick way to reapply sunscreen on kids at the beach or park, but can be avoided at home.
Fore more reading on sunscreen, see this post by two dermatologists who give their own advice, but geared towards adults, click here.
A lot of people are wondering about vitamin D. Although our skin can make vitamin D by being exposed to UVB light from the sun, the amount of sun it takes is variable by region and skin type, and enough sun to make enough vitamin D will also increase skin aging/wrinkles and cancer risks, so I still recommend using sunscreen, then getting vitamin D in your diet. For more information, see
http://www.vitamindcouncil.org/about-vitamin-d/how-do-i-get-the-vitamin-d-my-body-needs/
Do not use combination insect-repellent and sunscreen mixes. Insect repellents should not be applied more than once per day, and should not be applied to babies. For more information on insect repellents see here and here.
I used to link to the Environmental Working Group's sunscreen ratings, but their methodology has been ignoring science, and based on fear-mongering lately, so I stopped. For more information on that, see here and here.
EWG also warned against "nano particles" with no scientific basis. For information on them see this article from cancer.org.
*Here are some examples of sunscreens that use barrier (mineral) ingredients, in alphabetical order:
Aveeno Mineral Block
BabyGanics Cover-Up Baby Pure Mineral Sunscreen Stick
Banana Boat Natural Reflect Sunscreen
Burt's Bees Baby Bee Sunscreen
California Baby Sunscreen
Mustela Sun Cream and Sun Lotion
Neutrogena Baby Pure and Free
 |
| Here my son demonstrates proper beach attire with sunscreen (c) 2011 |






.jpg)